Rosacea can be frustrating because it is so multi-faceted, involving bright redness, dilated vessels, big pores, photosensitivity, extreme dryness and large cysts or acne — and possibly, all at the same time.
There is strong evidence that rosacea is more common than once thought. Rosacea is frequently under-diagnosed or misdiagnosed and its multi-factorial nature suggests that rosacea may share common inflammatory pathways with other inflammatory skin conditions. The contradictory nature of some symptoms — acne and severe dryness — can make treatment difficult (many acne treatments are drying on purpose, for example). There is clearly a need for a better understanding of rosacea.
We asked our founding dermatologist-dermatopathologist for help….
What Is Rosacea?
Rosacea is the prototype of red facial skin. It is characterized by:
- Centrofacial redness,
- Fine to more prominently-dilated capillaries (telangiectasia),
- Small bumps that become larger that may eventually develop into acne and thick skin.
One or more of the following is/are sufficient to make the diagnosis:
- Flushing (transient erythema or redness),
- Persistent redness,
- Obvious dilated capillaries,
- Papules (bumps without infected matter) or pustules (bumps with infected matter, like pimples).
Additional symptoms and signs to look for are: burning/stinging, facial edema (swelling), dryness, plaques (raised patches), eye redness, similar changes beyond the face, and phymatous (swelling, masses, or bulbous) changes of the nose.
Who Gets It?
Rosacea changes are often first seen at age 30, more among women, with men more often having the type that produces bulbous thickening (rhinophyma) of the nose and bumps. While rosacea is described as more common in fair-skinned individuals, there are no prevalence studies among Asians and darker skin types where it is known to exist but is also often unrecognized or misdiagnosed as contact, photocontact, seborrheic or atopic dermatitis.
Risk Factors/Causes
Those who tend to get rosacea seem to have a combination of 1) genetic predisposition, plus 2) an environment/lifestyle that includes triggers like spicy foods and sun and light exposure, 3) certain microbes on the skin and/or in the stomach, and 4) higher-than-normal levels of naturally-occurring pro-inflammatories in their bodies. In detail, common risk factors include:
- A tendency to flush (turn bright red) easily in response to:
- Certain chemicals or natural ingredients,
- Some foods, such as alcohol or hot (both temperature and spiciness) foods;
- Psychological factors like stress or shame.
- Chronic sun and light (including heat) exposure; and
- Genes: having blood vessels that increasingly dilate as they respond to stimuli.
Other factors include micro-organisms:
- Demodex folliculorum (mites that live in the hair follicles of susceptible people).
- Helicobacter pylori infection in the digestive tract.
Another theory concerns vascular development, the flow capacity of blood vessels, and neuro-transmitter mechanisms.
Some of the newest research shows cathelicidins as the primary cause for the inflammation in rosacea. These proteins are important to our innate immunity but are also PRO inflammatory. Cathelicidins are markedly increased in skin with rosacea which makes it hyper-reactive.
Our Recommendations:
Articles contributed by doctors do not contain product recommendations for ethical reasons, and we at VMV Hypoallergenics believe in protecting the integrity of our resource physicians. Below are some products that we at feel can be recommended based on the preceding resource information. They are our “skinformed” selections based on the insights given above and not necessarily recommended by the medical author of the article.
Most rosacea treatments use steroids or azelaic acid to reduce inflammation and redness, both of which are not intended for long-term use and can be irritating or have other side effects. Other treatments rely solely on antioxidants, and several contain allergens which are proven to promote inflammation and dryness. We recommend…
Prevention
The best way to deal with redness is to prevent it. Prevention is important in all health concerns. When it comes to rosacea and hyperreactive skin, it is vital. Your new mantra: “non-inflammatory”.
- Get 7-8 hours of sleep, de-stress, and exercise regularly (daily, even if some days are just easy walks).
- Improve your diet: avoid processed foods, white sugar, white rice, white pasta (switch to brown, whole-grain, and raw alternatives), soda, pre-packaged juices (even “health” juices), candies, and chips.
- Choose very gentle, non-reactive, anti-microbial and anti-inflammatory products in all of your personal care:
- Hair and body washing: Essence Skin-Saving Clark Hair & Body Wash and Conditioner.
- Sun protection: Armada Baby 50+ or Armada Post-Procedure Barrier Cream 50+.
- Makeup: Skintelligent Beauty.
Therapy
Try steroid-free, anti-inflammatory, moisturizing, comforting Red Better Redness + Inflammation Calming System.
STEP 1: Red Better Deeply Soothing Cleansing Cream (nay, custard) is an ultra-gentle, comforting facial wash.
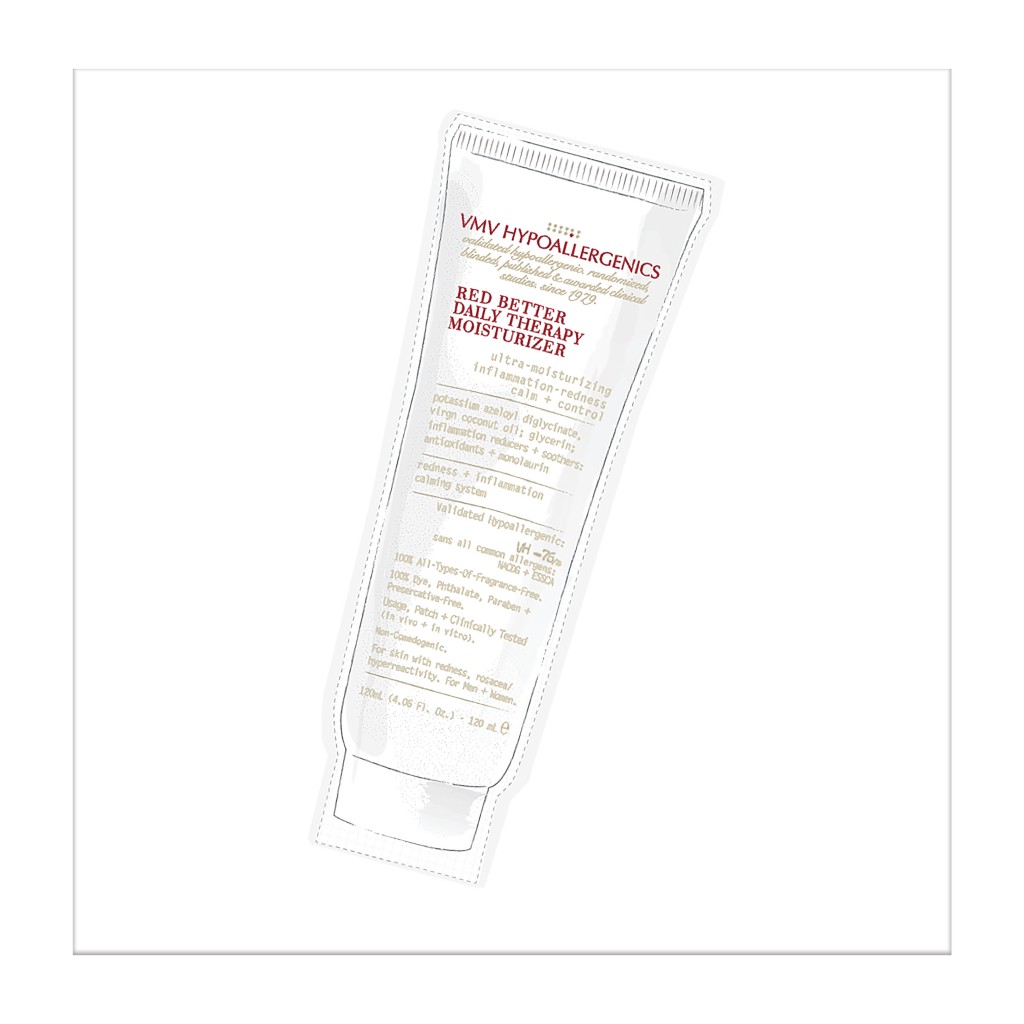
STEP 2: Red Better Daily Therapy Moisturizer for anti-inflammatory + anti-cathelicidin therapy plus rich, palliative yet non-pore-clogging hydration.
STEP 3: Armada Post-Procedure 50+, a purely physical (“inorganic”) sun + light screen for use both indoors and outdoors all year round. Redness conditions can be photosensitive and can flare up just from indoor light exposure. Its subtle (mineral) green tint offsets redness, too.
AS NEEDED: If you have acne, Red Better Spot Corrector is a uniquely non-drying (even hydrating and soothing!) quick-acting spot treatment. For flare-ups, try Red Better Flare-Up Balm.
FAN TIP: Keep your skincare in the refrigerator (especially soothing for red, hyperreactive skin)!
Red Alert Skin-Savers
The big deadline got moved up. Your toddler decided to see if your phone could swim. That curry was spicier than you thought. You’re finally meeting that big client after months of wooing. Despite your best efforts, this is too much for your skin and it happens: the full-scale(y), fire-engine-red flare-up.
Your doctor might prescribe a topical steroid for short-term use — follow these orders. But if you can’t get to your doctor, get relief with non-steroidal, non-irritating Red Better Flare-Up Balm.
Other skin-emergency tips:
- Dab Boo-Boo Balm on the tip of a wet towel wrapped around ice. Apply gently as a cold compress.
- If it’s such a bad flare-up that plain water stings, stop all products for the duration of the flare-up. Favor darkness (turn off lights and avoid windows). Meditate, sleep, relax — self soothing is important to not feed the inflammatory eruption. And see your dermatologist.
- If the reaction seems worse than a typical flare-up and you notice a rash that is spreading or difficulty breathing, get to the emergency room.
“Dew” More:
To shop our selection of validated hypoallergenic products, visit vmvhypoallergenics.com. Need help? Leave a comment below, contact us by email, or drop us a private message on Facebook.
If you have a history of sensitive skin, don’t guess: random trial and error can cause more damage. Ask your dermatologist about a patch test.
Learn more:
About rosacea, see Can’t Calm Rosacea? #candew!and Put Angry Skin On “N-ice”.
To learn more about the VH-Rating System and hypoallergenicity, click here.