With more and more research (finally!) into perimenopause and menopause, women are learning ways to relieve a wider range of symptoms and stay healthier, longer.
First: What’s What?
Menopause is defined as not menstruating for one year and the time thereafter. Perimenopause lasts years, even decades, often starting at age 47 but sometimes as early as 35.
Due to its many hormonal shifts and drastic drop in estrogen — and that estrogen receptors are present throughout the body — perimenopause comes with many more symptoms than mood swings and hot flashes (more correctly referred to as vasomotor symptoms). These include, but are in no way limited to, night sweats, joint and shoulder problems, depression, bone density, weight gain, muscle mass, vaginal dryness, cardiovascular health concerns, libido issues, and interrupted sleep.
A visit to your gynecologist, endocrinologist, and other specialists is important.
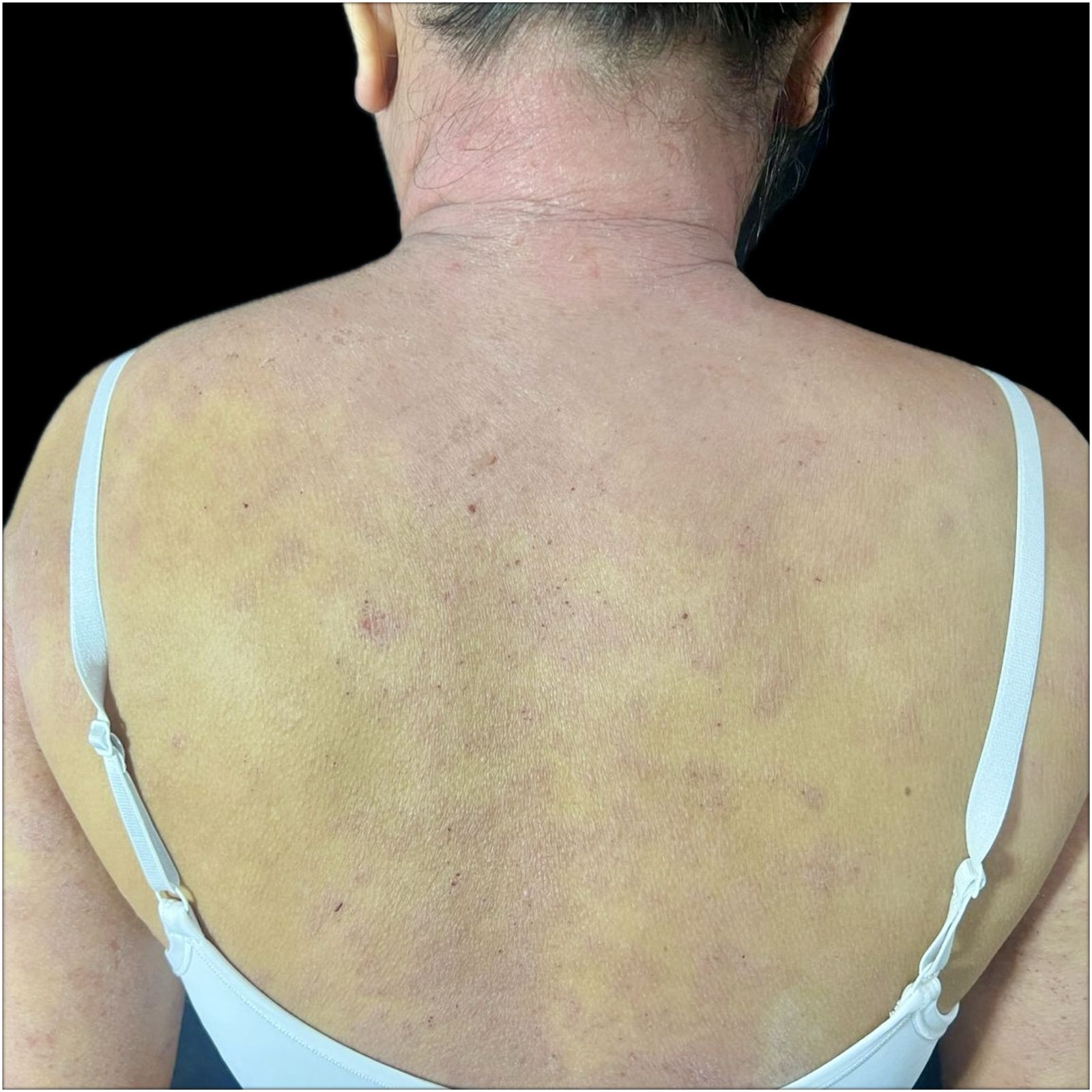
How Does Perimenopause Impact the Skin?
Perimenopause’s drastic reduction in estrogen can impact the skin in many ways, from the top (epidermis) to the glands and hair follicles, including:
- Dry, thinner skin which can also lead to:
- Increased sensitivity to ingredients and other substances
- Easier bruising
- Itchy skin feeling (or actual itching from irritations or allergic reactions due to increased skin sensitivity)
- Acne
- Hair growth on the face
- Hair loss on the head
- More signs of photoaging, such as dark spots and blotches
- Less collagen in the skin (we lose around 30% within the first 5 years of menopause) means more sagging, thinning, crepe-like texture, and wrinkles
- Increased risk of skin cancer (which could also be from aging and increasing exposure)
- Red skin from hot flashes
- Change in body odor (or change in sense of smell making us think body odor has worsened)
- Vaginal dryness, irritation, and some more common vaginal infections
What Can Help Perimenopausal Skin Issues?
- See your dermatologist.
- See your gynecologist and ask about hormone replacement therapy (HRT), especially if you’re 60 years old or younger and within 10 years of the start of menopause.
- Estradiol and Estriol (topical estrogen) applied to the vagina.
- Some research suggests that virgin coconut oil can also provide relief as effective as some ECT (estrogen containing therapies) and without adverse reactions. This one study included pre and postmenopausal women with vaginal dryness and dyspareunia (VDD), with and without Rheumatic Autoimmune Diseases such as primary Sjogren’s syndrome, where VDD is a common symptom. Ask your gynecologist and dermatologist.
- Choose skincare, hair-body care, and makeup that’s allergen-free, non-comedogenic, non-acnegenic — with all those possible skin symptoms (from increased sensitivity to acne and hair loss, safety is your best friend!)
- Prioritize barrier care: choose hypoallergenic moisturizers that feature virgin coconut oil.
- If your skin is very, very dry or barrier deficient, consider layering. Start with any of our moisturizers, then follow with our virgin coconut oil Know-It-Oil or Oil’s Well. End with Boo-Boo Balm for more occlusion.
- Daily sunscreen, even when indoors (UVA can go through windows and blue light/visible light can cause hyperpigmentation).
- Due to the increased dryness and sensitivity, you might want to consider a product that locks in more moisture and is more opaque, such as Stay-On-Point! (Armada Post-Procedure).
- Fragrance-free, whole-body deo Essence Stay Fresh-ener or Essence Antiperspirant for body odor and sweating. Try applying on more places like the back, behind the knees, etc. and reapplying before sleep for hot flashes at night.
- Apply Id Monolaurin Gel after Essence if you need more odor control.
- Bring Essence or and/or Id with you to reapply during the day.
Subscribe to VMVinSKIN.com and our YouTube channel for more hypoallergenic tips and helpful “skinformation”!
If you have a history of sensitive skin…
…don’t guess! Random trial and error can cause more damage. Ask your dermatologist about a patch test.
To shop our selection of hypoallergenic products, visit vmvhypoallergenics.com. Need help? Ask us in the comments section below, or for more privacy (such as when asking us to customize recommendations for you based on your patch test results) contact us by email, or drop us a private message on Facebook.
For more:
- For a video on hyperhidrosis and bromhidrosis: Bad Body Odor & Sweating
- On hyperhidrosis and other conditions that can be embarrassing, see “Skintimate” Problems: Skin Issues Related to Underwear, Sex & Other Things That Might Embarrass You (But Shouldn’t).
- On monolaurin, see Study Review: Coconut Oil, Monolaurin & Other Derivatives As Antivirals.
- To learn about the VH-Rating System and hypoallergenicity: What Is The Validated Hypoallergenic Rating System?

Laura is our “dew”-good CEO at VMV Hypoallergenics and eldest daughter of VMV’s founding dermatologist-dermatopathologist. She has two children, Madison and Gavin, and works at VMV with her family and VMV’s signature “skinfatuated, skintellectual, skingenious” team. In addition to saving the world’s skin, Laura is passionate about health, cultural theory, human rights, happiness, and spreading goodness (like a VMV cream)!